Effect of endobronchial valves on the lungs
Endobronchial valves are inserted under general anaesthesia with the help of a delivery catheter into the central airways of a pulmonary lobe. These valves are the size of a thumb tip (4-8 mm) and serve to close the afferent bronchi of the pulmonary lobe which is most affected by the hyperinflation of the alveoli. As a result, no further air can enter the blocked portion of the lung area during inhalation, but secretions and air are allowed to escape (valve effect). The ventilated/affected area of the lung shrinks and there is a tendency for it to collapse (pulmonary collapse). Whether the lungs of the COPD sufferer are suitable for implantation of the valves has to be determined by means of a special test. Less than 50% of the tested COPD sufferers are said to be suitable for the valves.
After receiving valve implants, many patients report coughing out some of the valves during expectoration. Valves can be removed again at any time.
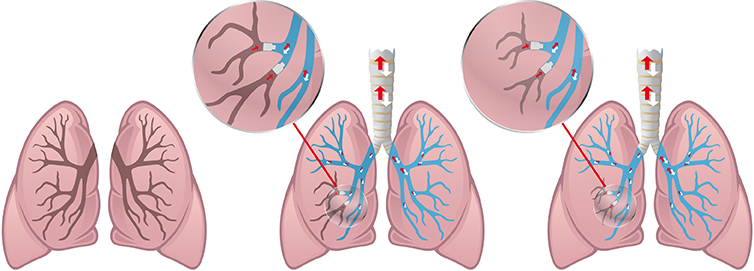
Two endobronchial valves are inserted in the middle branch of the left lung. Only air and gases can escape from the area behind the valves. The valves prevent new air from entering this area. No longer supplied with new air and oxygen, this lung/branch becomes smaller and stunted.
To summarise:
COPD sufferers are advised/prescribed a wide variety of COPD medications to be taken on a daily basis over a period of years, medications that result in or actually cause hyperinflation of the alveoli. When pulmonary emphysema is then present and COPD drugs cannot hyperinflate any more, surgical methods such as endobronchial valves or coils are recommended to reduce or contract the hyperinflated lung tissue, something that permits hyperinflation in other areas of the lung. This is a very curious logic that we fail to grasp and that contradicts biological logic.
An honest and open discussion with sufferers who have had valves or coils in their lungs for weeks and months (long-term experience) can help patients make their own decision for or against such surgical procedures.
Remark:
Classic COPD drugs have a sympathicotonic effect. This means that already stressed COPD patients are artificially subjected to even more (permanent) stress. This works to expand — or, to be more exact, to hyperinflate — the alveoli and bronchi even more, and this day after day. Such therapy makes it biologically impossible for repair and regeneration processes to take place in the lung tissue!
